The new exciting content of BSG web education is live. Challenge your diagnostic skills and learn from the experts in the field! Endoscopy case series and Bite Size take you through a patient’s case and offer concise and up-to-date knowledge on less common conditions. #takethechallange #takeabite
Dr Miles C Allison, Consultant Gastroenterologist, Aneurin Bevan University Health Board, Newport, NP20 2UB, South Wales.
Introduction
A 78-year-old woman with no relevant past history presented acutely with right upper quadrant pain. CT demonstrated a large stone in the neck of a thickened gall bladder (Figure 1a). She received intravenous antibiotics and was discharged with a view to elective laparoscopic cholecystectomy.
Five months later, she was re-admitted with further pain and weight loss. CT was repeated (Figure 1b).
Question 1
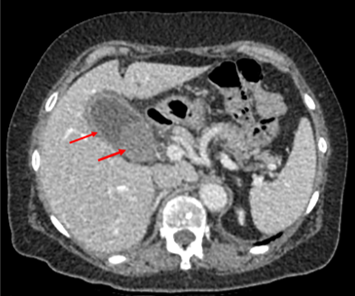
Figure 1a

Figure 1b
She then developed haematemesis requiring a 4-unit blood transfusion. Gastroscopy showed a pool of altered blood in the stomach and a fresh blood clot emerging from the pylorus. A large ulcerated area was found in the proximal second part of the duodenum (medial wall – Figure 2).
Question 2

Figure 2
The second CT demonstrated air in the gall bladder and biliary tree. A large stone had fistulated from the gall bladder neck into the second part of the duodenum and had become impacted in the third part of the duodenum (Figure 3). Thus haematemesis was due to a combination of bleeding from the fistula and distal duodenal obstruction from the stone (Bouveret’s syndrome). The bleeding point was managed with adrenaline injection and the application of Haemoclips (Figure 4).
Question 3

Figure 3

Figure 4
Electrohydraulic lithotripsy is unlikely to succeed given the size of the stone. The patient had already undergone a prolonged procedure to manage the bleeding, so a direct rapid approach was attempted. It was possible to engage the stone in an ERCP mechanical lithotripsy basket (BML-V242QR-30 Olympus) under direct vision and withdraw it to the cardia, but it would not crush and it was too large to come up through the gastro-oesophageal junction. The lithotripsy catheter and wires were severed with a wire-cutter outside the endoscope. The latter was withdrawn, and a rescue lithotripter was applied to crush the stone in the stomach. At repeat gastroscopy the stone had reduced in size and was re-engaged using another lithotripter basket. On this occasion it proved possible to withdraw the stone up the oesophagus and out through the mouth (Figure 5).
The patient tolerated the procedure well, although she complained of sore throat for 72hr. She received an intravenous infusion of Omeprazole during this time and was discharged four days post-procedure.
Question 4

Figure 5
Discussion
Bouveret’s syndrome was first described by Léon Bouveret in 1893 in Revue de médecine, where he reported two cases of this syndrome. Gastric outflow obstruction occurs secondary to gallstone impaction in the duodenum due to migration of a large stone via a cholecysto-duodenal fistula (1). Bilio-enteric fistulae develop from chronic cholecystitis and adherence of the inflamed gall bladder to the bowel. There may be active ulceration at the fistula site, and submucosal ischaemia may develop as the stone penetrates the duodenal wall. The female: male incidence of this complication is 1.9: 1 (2). This higher frequency in older women (median age of 74 years) may simply reflect the prevalence of gallstone related complications in this patient group. It accounts for about 2% of cases of gallstone ileus, in which large stones much more commonly obstruct the distal ileum (3).
Typically, patients present with a short history of nausea and vomiting, sometimes with associated abdominal pain and weight loss. Haematemesis with or without melaena complicates the picture in 15% of cases (3).
CT scanning usually demonstrates air in the biliary tree and the presence of a large gallstone impacted in any part of the duodenum, most often at the pylorus or in the duodenal bulb (2). Gastroscopy can demonstrate the site of the obstruction, and may provide an opportunity for therapy.
It can be very challenging to advance accessories such as snares or Roth nets beyond the obstruction to allow the impacted stone to be grasped and pulled back into the stomach. Mechanical lithotripsy using ERCP baskets can be used to crush the stones (4,5). Laser and electrohydraulic lithotripsy have become popular more recently (3,4). Impaction in the distal duodenum and maximum stone length are factors which predict failure of endoscopic therapy (5). In my own experience, dense solid stones are less likely to respond to lithotripsy than softer lighter stones. Every effort should be made to capture and retrieve the stone or its fragments via the mouth to prevent the development of gallstone ileus further down the small intestine.
Surgical approaches include duodenotomy, pylorotomy or gastrotomy, milking the stone into the stomach (2,3). The outcome of this conservative approach is at least as good as that of cholecystectomy and fistula repair, though numbers of reports are small (2). Gallbladder malignancy is occasionally found to underly Bouveret’s syndrome, but the large majority of cases are benign and occur in older age groups. An attempt at cholecystectomy is recommended in younger fitter patients because cholecysto-enteric fistula may predispose to malignant transformation.
Author Biography
Dr Miles C Allison
Dr Allison trained in gastroenterology and hepatology at the Royal Free Hospital, London, and in Glasgow Hospitals. He has been a consultant physician with a special interest in gastroenterology in South Wales since 1991. He served on the BSG Endoscopy Committee for six years from 2002 and was lead author on guidelines for decontamination of endoscopes, antibiotic prophylaxis for GI endoscopy and risk avoidance for variant CJD. He was founder secretary of the Welsh Association for Gastroenterology and Endoscopy and was Professional Lead in the establishment of Bowel Screening Wales.
CME
Newly formed ATSMs in ERCP and BSCP
24 November 2025
National Clinical Endoscopists Conference 2025 Recording
13 November 2025
Quality Indicators in Barrett's Endoscopy: A Quest for the Holy Grail
27 October 2025
- Bouveret L. Traite des maladies de l’estomach (Textbook on diseases of the stomach). Paris: Bailliere et fils, 1893.
- Cappell MS, Davis M. Characterization of Bouveret’s syndrome: a comprehensive review of 128 cases. Am J Gastroenterol 2006; 101: 2139-46.
- Caldwell KM, Lee SJ, Leggett PL, Bajwa KS, Mehta SS, Shah SK. Bouveret syndrome: current management strategies. Clin Exper Gastroenterol 2018; 11: 69-75.
- Dumonceau J-M, Deviere D. Novel treatment options for Bouveret’s syndrome: a comprehensive review of 61 cases of successful endoscopic treatment. Expert Rev Gastroenterol Hepatol 2016; 10: 1245-55.
- Ong J, Swift C, Stokell BG et al. Bouveret syndrome: a systematic review of endoscopic therapy and a novel predictive tool to aid in management. J Clin Gastroenterol 2020; 54: 758-68.
