Author:
Alan Lobo, Consultant Gastroenterologist and Professor of Gastroenterology
Introduction
Services need to be configured to match complex needs of people with Inflammatory bowel disease (IBD). Personalised care is part of The National Health Service (NHS) Five Year Forward View. IBD Standards (IBD UK, 2019) emphasise personalised care throughout the patient pathway and IBD UK’s National Report (2021) identifies key areas for change:
- Diagnosis and information
- Personalised care and supported self-management
- Access to specialist advice
- Multidisciplinary working
The AWARE-IBD programme (Chief Investigator, Professor Alan Lobo) addressed these challenges -focused on ‘What matters to you?’ - between 1.3.2021 and 15.2.2024, led by patients. We used their experience and values to co-produce changes with quantitative and qualitative evaluation (Figure 1).
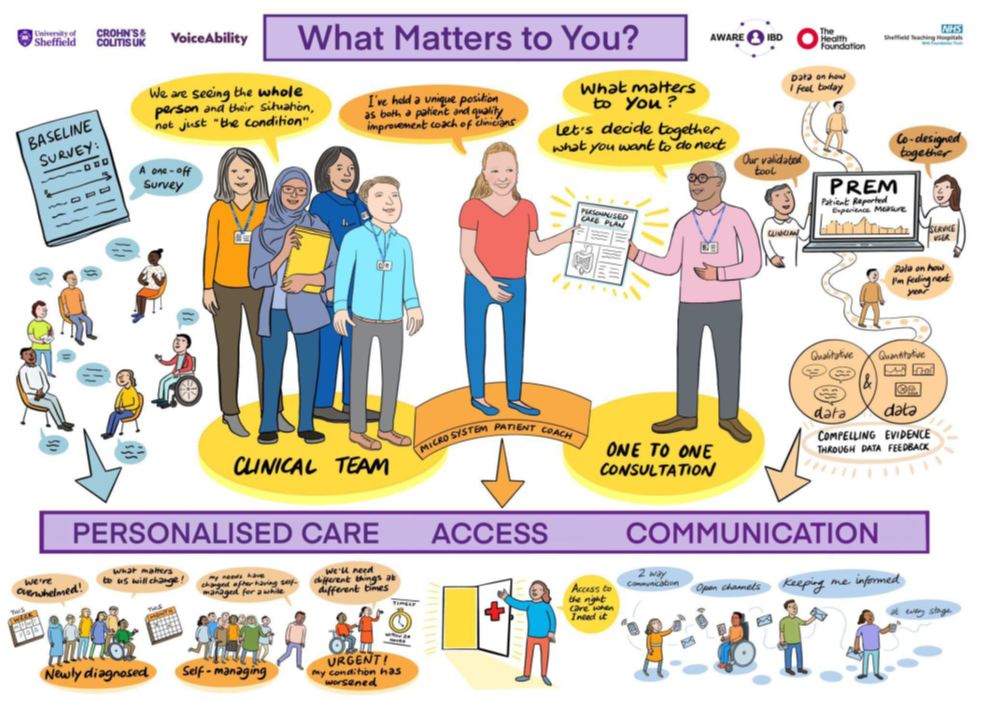
Figure 1. The AWARE-IBD project - overview
Why we needed to change?
- Patients making a difference in quality improvement (QI) is an NHS priority.
- Patients (Survey 2021; n=613) identified priorities:
- Access
- Communication
- Personalised care
- IBD Standards also recommend the use of a personalised care plan (PCP) but with no agreement on what this comprises
- Delays for people requiring urgent review. Timely clinic appointments were unavailable for those calling the help-line, which puts pressure on nurses taking calls.
- Newly diagnosed patients described poor access and information.
- Engagement of people from under-served communities was limited.
- There was no instrument to measure patient experience of an IBD service.
Overcoming the challenges
1. Patient Leadership and Partnerships
- Patients were leaders and partners:
- A Microsystem approach was adopted, led uniquely by a patient coach.
- Two additional patients participated in the microsystem - on equal terms with clinicians.
- The national patient charity, Crohn’s & Colitis UK (CCUK), were a named partner.
- The project team were accountable to a Patient Oversight Committee, chaired by CCUK.
- Underserved communities characterised by deprivation, ethnicity, disability (deafness) and sexuality (LGBTQ+) were engaged in 11 meetings.
- Delivered by partnership of multidisciplinary clinical team, CCUK, health researchers, and VoiceAbility (peer support organisation).
2. Measuring experience
- Co-designed new Patient Reported Experience Measure (PREM) using Capability, Opportunity, Motivation (COM-B) framework - published and prospectively validated covering 3 domains. Recruitment from two cohorts:
- Everyone attending IBD service.
- Follow-up letter and targeted contact with deprived population deciles and ethnic minority groups.
3. Access
- Specific clinical groups (new IBD, flare, new biologic) were prioritised in dedicated, specialist consultant clinics in improvement cycles.
4. Personalised Care
- New co-designed IBD PCP (survey (n=130), 2 workshops) included “What matters to you?”
5. Communication
- IBD Patient Toolkit: co-designed to support confident communication and build skills for self-advocacy (available in paper form, online (voiceability.org/aware-ibd) in multiple languages and EasyRead™).
- IBD Education Programme: content and format co-designed. Eight sessions delivered at local venues by IBD team and patients.
Outcomes
- 279 patients completed the PREM between November 2021 and November 2023. Patient experience improved significantly overall (increase 0.17 points (0.95 CI 0.12 – 0.23; p<0.001)), across each domain and in both cohorts (Figure 2). The increase was greatest in those diagnosed in the last five years (mean increase 0.3 points (p=0.001)).
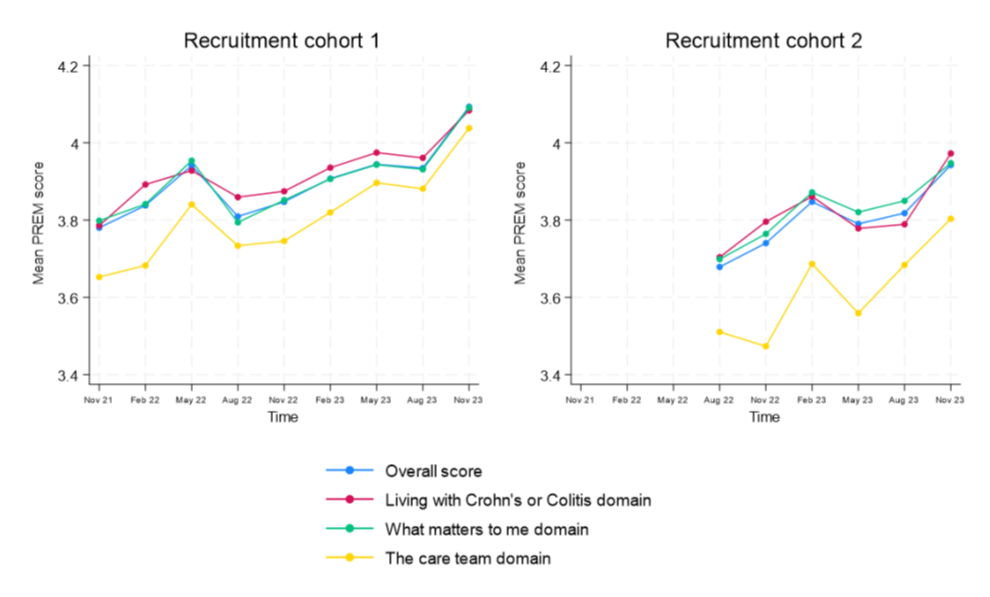
Figure 2. Change in mean PREM score during AWARE-IBD programme.
- PREM improved most in those with worse experience at baseline (mean increase over two years for those in lowest third of baseline scores: 0.49 points (0.95CI: 0.36 to 0.61) v 0.16 (0.95CI: 0.08 to 0.24) for those in middle third; no change for highest third.
- PCP was used in 67 consultations. Base-line PREM was already high in this group (median 4.08 (max 5)). Experience in the care team domain improved but effect size was small (increase 0.21 points (0.95 CI 0.03 – 0.38; p=0.019)), greatest in the three most deprived deciles (mean increase 0.52 points (p=0.03)); “It made me ask the difficult questions I shy away from … about where I am on the journey.”
- Patients in consultant priority clinics were seen more rapidly with reduced variation in interval to be seen. For example, time (days) to be seen reduced for those with suspected flare, (median baseline 76; Tests of change median 1-2) with markedly reduced variation (Figure 3). Time to initiate treatment was not reduced.
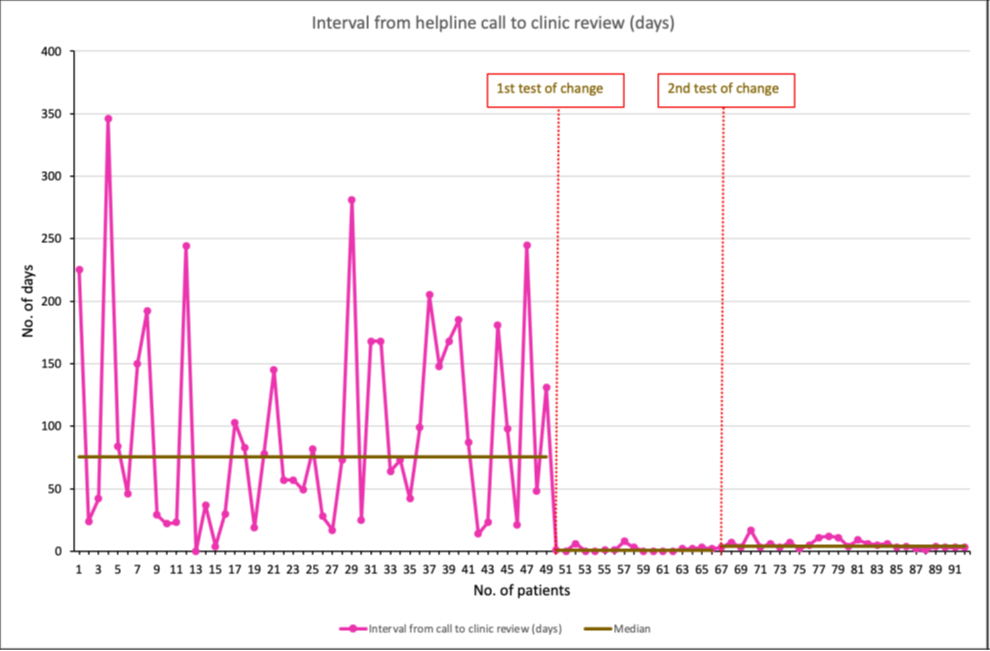
Figure 3. Change in interval (days) from helpline call to clinic review during AWARE-IBD programme.
- In semi-structured interviews, benefits and limitations were reported by staff and service users:
- Rapid access to detailed discussion with specialists.
- Reduced pressure dealing with calls to the helpline because an urgent appointment was available.
- Nurses staffing the helpline still needed to manage available capacity, requiring judgement about allocating specialist appointments.
- Education sessions: attendees reported positively on breadth, quality and - unexpectedly - peer support.
- IBD Patient Toolkit: viewed online 685 times, by 370 unique users (05.06.2023 - 08.02.2024). “…this project has made me use my appointments more effectively … I am more proactive” (Toolkit user).
- Patient panel established to sustain patient leadership of QI.
Learning
- Patient experience reflects service delivery. A new, co-designed, published IBD PREM allows measurement of experience and comparison over time and across centres.
- Participation in an extensive QI programme was associated with significantly improved experience over two year follow-up. Effect size was modest - though a high baseline may have limited potential for improvement.
- Barriers to engagement in underserved communities included service accessibility, language, literacy, advocacy, being dismissed, lack of continuity, mental health and social support.
- Development and implementation of a PCP produced benefits, particularly in deprived deciles, allowing more widespread, longer-term adoption and evaluation.
- IBD services are a complex adaptive system with a dynamic interplay of capacity, demand, staffing, expertise, need for continuity, alternative pathways, local and national priorities causing variation in access. QI initiatives require detailed ‘buy-in’ from managerial, clerical and clinical teams to reconcile these.
Conclusion
- Evidence-based care incorporates best evidence, clinical perspective and patient values. These values can be systematically sought and respected in service design.
Read More

