BSG CSSC Service Development Prize 2023 joint 3rd place submission by Dr Chirantha Premathilaka
Names of team involved:
Chirantha Premathilaka1,2, Pauline Dundas2, Nicola Beech2, Lorna Bailey2, Shirley English2, Lindsay McLeman2, Chaitra Chandra Shekar2, Balasubramaniam Vijayan2, Ashis Mukhopadhya2
1University of Aberdeen
2NHS Grampian
Introduction – the challenges to our service
Cirrhosis is an increasingly prevalent condition associated with significant morbidity and mortality. When these patients have unscheduled admissions following decompensation, readmissions rates, lengths of stay, and mortality can be very high. Ideally, factors leading to decompensation like diuretic dose or laxative treatment would be optimised to prevent admission in the first place but the reality is that it is difficult for consultants with lengthening outpatient waiting lists to prioritise patients that would benefit the most from enhanced monitoring. This all contributes to a growing burden on healthcare systems. Thus, the challenge is to develop a resource-efficient solution to manage this cohort.
Methods – the strategy we developed and how we evaluated effectiveness
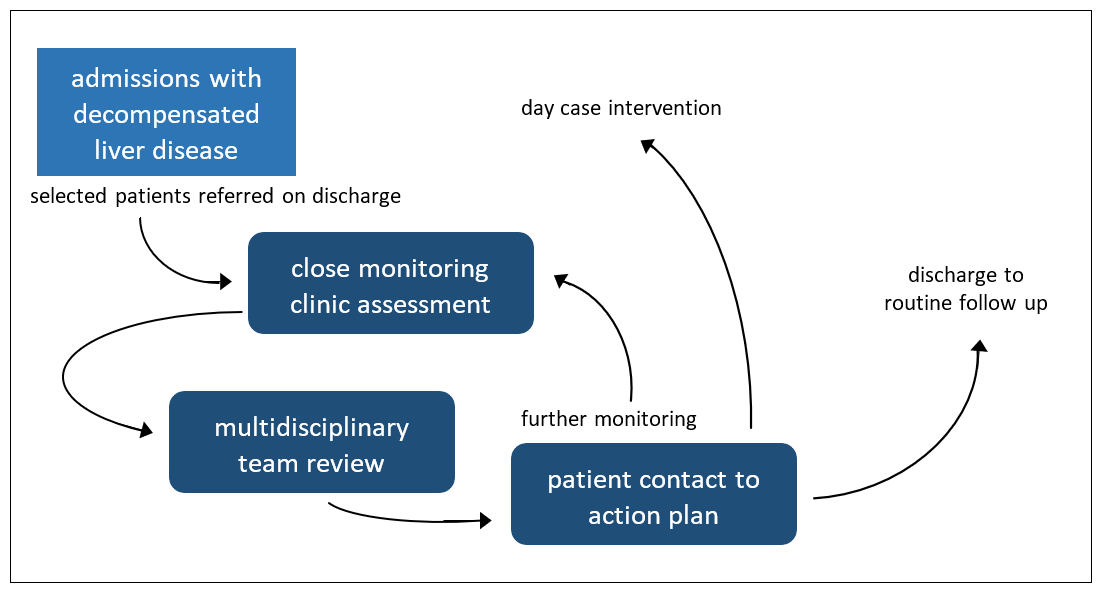
In 2019, the close monitoring clinic was set up in Aberdeen Royal Infirmary with aim of supporting patients with decompensated liver disease post-discharge. On discharge, consultants highlight patients for follow up in the close monitoring clinic based on clinic assessment of likelihood of decompensation. These selected patients are reviewed in 1-2 weeks at an outpatient specialist nurse-led clinic whose staff can examine perform clinical examinations, routine tests, modify prescriptions, and organise day case drains. It is further supported by a multidisciplinary team meeting attended by hepatology consultants who provide advice the following day. After multidisciplinary team review, patients are telephoned to action plans, e.g., diuretic doses, laxative changes, electrolyte management.
-nurse-pathway-for-decompensated-liver-disease.png)
Figure 1. close monitoring clinic pathway
In order to assess our impact, we performed a retrospective analysis of the case mix at our site between 2018 and 2022 to determine if there was a difference in the readmission rates, lengths of stay, and mortality rates of the patients who attend the close monitoring clinic compared to those who did not. The cases were identified using ICD-10 discharge codes encompassing decompensated liver disease.
Results and Discussion – impact on outcomes
The mean number of admissions with decompensated liver disease each year was 136. On average, readmissions comprised 59% of total admissions.
The close monitoring clinic had 560 appointments with 203 unique patients between 2019 and 2022, averaging 140 appointments and 59 unique patients per year.
-nurse-pathway-for-decompensated-liver-disease.png)
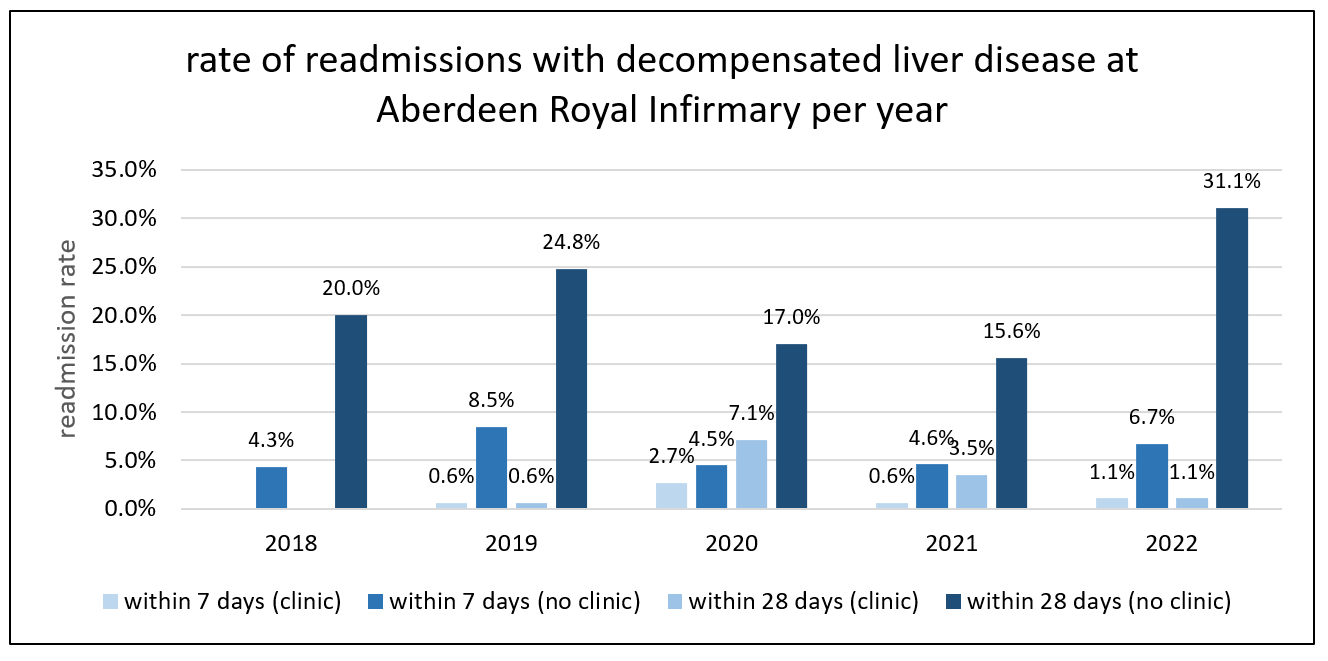
Figure 2. 7 and 28 day readmission rates for patients discharged from Aberdeen Royal Infirmary with decompensated liver comparing those who attended close monitoring in the last year with those who did not
The 7 day readmission rate reduced significantly from 5.7% to 1.2% (mean difference: 4.5%, p<0.05) if a patient attended close monitoring clinic in the preceding year compared to if they had not. The 28 day readmission rate reduced from 21.7% to 3.1% (mean difference: 18.6%, p<0.05).
The average length of stay reduced significantly from 6.8 to 3.8 days (mean difference: 2.9 days, p<0.05) if a patient attended close monitoring clinic compared to if they had not.
-nurse-pathway-for-decompensated-liver-disease.png)
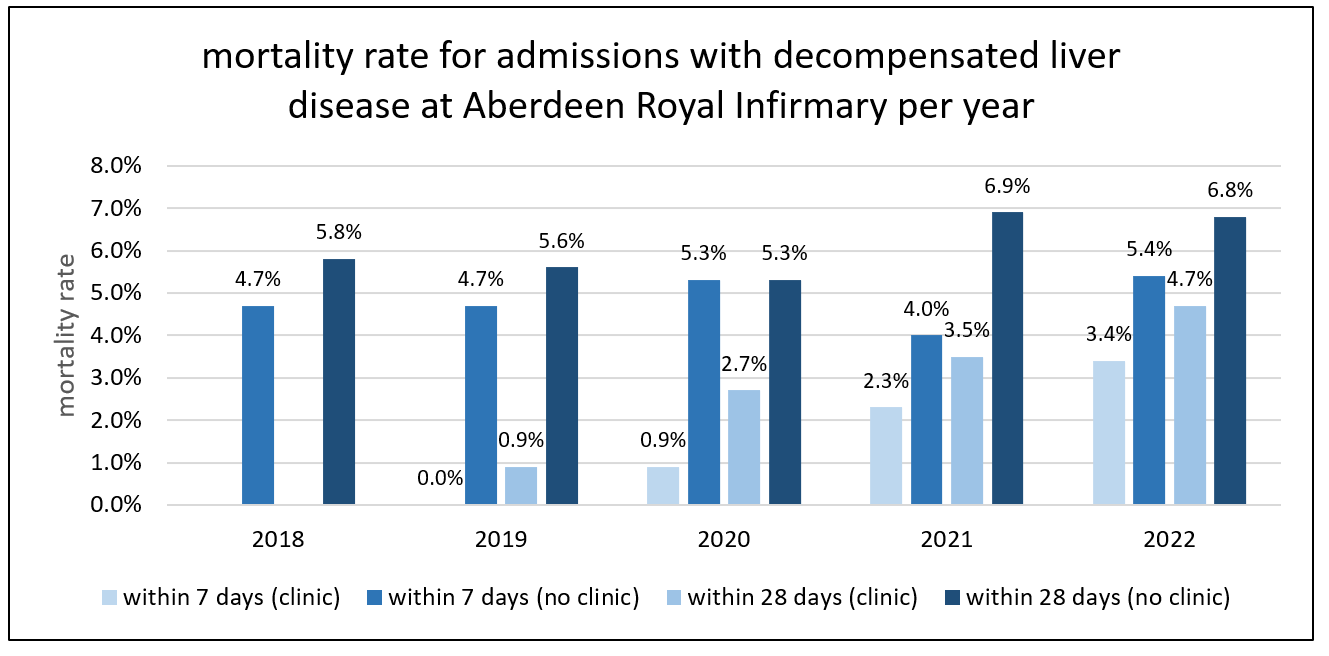
Figure 3. 7 and 28 day mortality rates for patients admitted to Aberdeen Royal Infirmary with decompensated liver comparing those who attended close monitoring with those who did not
The 7 mortality rate reduced significantly from 4.8% to 1.6% (mean difference 3.2%, p<0.05) if a patient attended close monitoring clinic compared to if they had not. The 28 day mortality rate reduced from 6.1% to 2.9% (mean difference 3.1%, p<0.05).
Overall, patients who attended close monitoring clinic had better outcomes compared to those who did not. There is a benefit in selecting patients for enhanced monitoring and targeting opportunities for interventions that can prevent admissions. The close monitoring clinic pathway accomplishes this efficiently and effectively while minimizing the burden on consultant time.
Conclusions – key learning points and messages for other sites
The close monitoring clinic is an effective intervention as regards reducing readmission, length of stay, and mortality. It also reduces the demand on hepatology consultant outpatient appointments. These improvements translate into fewer inpatient resources needed to care for this cohort and thus can be a cost-effective investment for healthcare systems.
This report describes a novel nurse-led post-discharge pathway that had a significant positive impact on outcomes for patients with decompensated liver disease. It would then be prudent for other healthcare systems to evaluate their own outcomes to determine if a similar model can be adapted to care to meet the needs of their cirrhotic population. In the future, the whole hepatology community stands to gain from sharing outcomes and strategies between sites to understand which interventions confer the greatest impact.
Read More

