Introduction
Fistulising perianal Crohn’s disease (pCD) represents a major issue for patients and has a cumulative risk of over 25% at long-term follow-up. The phenotype of rectal and perianal involvement in CD is predictive of a poor outcome, poses a significant psychological burden, and impacts on quality of life. Patients have a lot to lose if their disease is not controlled adequately and promptly. The disease course can ultimately culminate in the need for surgery, which might be a proctectomy and permanent ileostomy.
There is still a lot to learn about this phenotype of disease and various needs are unmet:
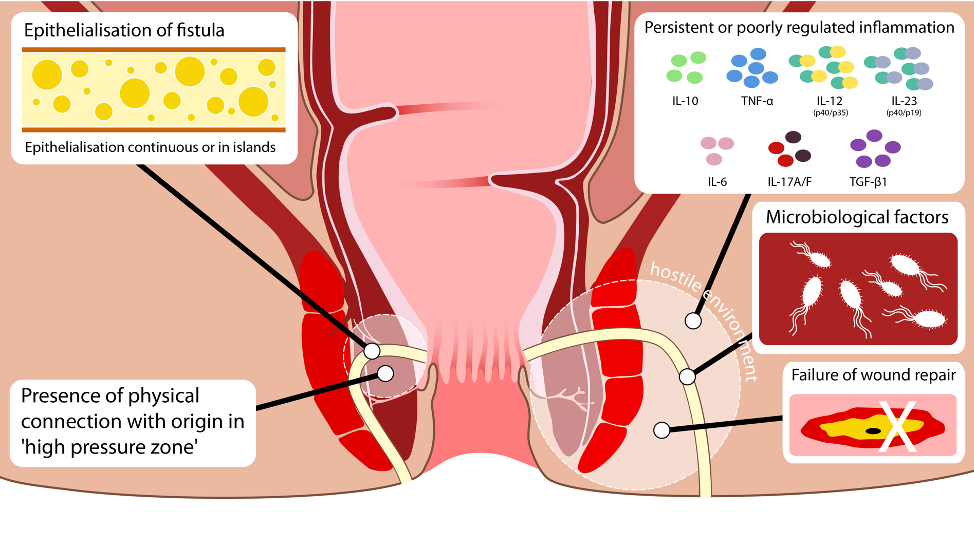
- Clearer understanding of the pathogenesis of fistulising pCD2, which is likely to involve not only factors associated with luminal disease (i.e. genetic predisposition and persistent poorly regulated inflammation, potentially due to microbial factors, with associated poor wound healing) but also physical and anatomical factors, such as the epithelialisation of the tract, the issue of an unfilled space that has a physical connection with the bowel lumen, and the presence of a high pressure zone.
- Sub-optimal classification of pCD6.
- A consistent definition of outcomes in pCD; a recent publication of a core outcome set that encompasses clinician-reported outcomes, patient-reported outcomes, and radiological outcomes should assist in future trial design to ensure that a common language is used[3].
Six-step guide to optimise managing this difficult form of CD
- Ensure a prompt diagnosis – remember that in 10% of patients perianal issues are the initial manifestation of pCD; in a very small proportion they are the only manifestation of pCD, so it is important to educate surgical colleagues and GPs, who are often the first to interface with these patients, to consider pCD if they see a patient with a perianal abscess.
- Multi-modal assessment is needed[1,6], usually with a combination of clinical history and examination, MRI, examination under anaesthesia, and endoscopy. The order of investigations can depend on local factors and availability, but the combination gives the optimum assessment of the disease. Newer techniques, such as three-dimensional imaging, can further help in evaluation[4].
- Recognising when psychological support is needed in this cohort is really important because pCD is associated with particular psychological morbidity. A new Crohn’s anal fistula quality of life scale is in development to help identify patients with pCD in the clinic and access support for them, as well as providing an important measure in trials.
- Combined medical and surgical approaches are needed to optimise care[1,5,6], usually involving examination under anaesthesia to drain any abscesses or insert a seton, followed by medical therapy with antibiotics and combination therapy with thiopurines and anti-tumour necrosis factor agents (anti-TNFs). Accumulating data indicate that increased serum levels of anti-TNFs are associated with improved outcomes and that this treatment combined with frequently repeated examinations under anaesthesia, local therapy with fistula tract laser closure and/or video-assisted anal fistula treatment (directed by optimal imaging to identify sub-optimally drained primary or secondary extensions) might improve management. Novel therapies, such as mesenchymal stem cells, offer other options.
- Monitoring the disease is important with use of careful clinical examination and MRI to support and assist in optimising the medical and surgical approaches[1,6].
- Finally, ensure that patients are educated about how to access the system of care, for example if they get an intercurrent abscess. Let patients know who to contact and how to contact the team.
Conclusions
For patients with pCD, ensure a prompt diagnosis is made so that patients can start appropriate therapy in a timely manner. Also ensure that optimum assessment is achieved by using a combination of clinical assessment, imaging, and examination under anaesthesia. Psychological support can be helpful for many patients with pCD who are struggling with a difficult burden of symptoms. Combined medical and surgical approaches are needed for disease management, and the pathway should include monitoring and optimisation of therapy. Patients need to be educated about their disease and, importantly, how to access the system if they have intercurrent issues.
Tozer et al. Aliment. Pharmacol. Ther. 2018 Aug;48(3):260-269
Author Biography
Dr Ailsa Hart
CME
IBD Surveillance Colonoscopy – This is how I do it
03 December 2024
SSG Digest This! Simulated multi-disciplinary meeting: IBD scenarios
16 October 2024
Masterclass - Chronic Pouchitis what you need to know
15 October 2024
- Gecse KB, Sebastian S, Hertogh Gd, et al. Results of the Fifth Scientific Workshop of the ECCO [II]: Clinical Aspects of Perianal Fistulising Crohn's Disease-the Unmet Needs. J Crohns Colitis 2016;10:758–765.
- Tozer PJ, Lung P, Lobo AJ, et al; of ENiGMA Collaboration. Review article: pathogenesis of Crohn's perianal fistula-understanding factors impacting on success and failure of treatment strategies. Aliment Pharmacol Ther 2018;48:260–269.
- Sahnan K, Tozer PJ, Adegbola SO, et al; the ENiGMA collaborators. Developing a core outcome set for fistulising perianal Crohn's disease. Gut 2019;68:226–238.
- Sahnan K, Adegbola SO, Tozer PJ, et al. Innovation in the imaging perianal fistula: a step towards personalised medicine. Therap Adv Gastroenterol 2018;11:1756284818775060.
- Sebastian S, Black C, Pugliese D, et al. The role of multimodal treatment in Crohn's disease patients with perianal fistula: a multicentre retrospective cohort study. Aliment Pharmacol Ther 2018;48:941–950.
- Gecse KB, Bemelman W, Kamm MA, Stoker J, Khanna R, Ng SC, Panés J, van Assche G, Liu Z, Hart A, Levesque BG, D'Haens G; for the World Gastroenterology Organization, International Organisation for Inflammatory Bowel Diseases IOIBD, European Society of Coloproctology and Robarts Clinical Trials. A global consensus on the classification, diagnosis and multidisciplinary treatment of perianal fistulising Crohn's disease . Gut. 2014 Sep;63(9):1381-92